Tobacco Smoke, E-cigarettes and Asthma
Tobacco smoke, whether you inhale from your own cigarette or breathe in secondhand smoke, is dangerous to your health. E-cigarettes may not be much better. When you have asthma, either type can be even worse.
What are E-cigarettes?
 Electronic cigarettes (e-cigarettes) is the name given to a group of battery-operated tobacco products that allow users to inhale aerosolized liquid (e-juice) that has nicotine and other substances. The terms “e-cigarettes” and “e-cigs” are often used for electronic cigarettes, as well as for e-pens, e-pipes, e-hookah, and e-cigars. These products are also sometimes called “JUULs” (after a branded e-cigarette of the same name), “vapes,” and “vape pens.” Unlike real cigarettes, e-cigarettes are made up of a battery-operated heating part — a cartridge (unit) that typically holds nicotine and other chemicals that change into a chemical-filled aerosol when heated.
Electronic cigarettes (e-cigarettes) is the name given to a group of battery-operated tobacco products that allow users to inhale aerosolized liquid (e-juice) that has nicotine and other substances. The terms “e-cigarettes” and “e-cigs” are often used for electronic cigarettes, as well as for e-pens, e-pipes, e-hookah, and e-cigars. These products are also sometimes called “JUULs” (after a branded e-cigarette of the same name), “vapes,” and “vape pens.” Unlike real cigarettes, e-cigarettes are made up of a battery-operated heating part — a cartridge (unit) that typically holds nicotine and other chemicals that change into a chemical-filled aerosol when heated.
How E-Cigarettes Might Affect Allergies and Asthma
The e-juice/liquid in e-cigarettes contains harmful substances that could trigger an asthma attack or worsen nasal allergy symptoms, either by the person using the e-cigarettes or even from a person breathing the ‘secondhand aerosol’ that comes from the e-cigarette. Breathing the aerosol from someone else’s e-cigarettes makes the risk of an asthma attack go up by 27%.
While much remains to be determined about the lasting heath consequences of e-cigarettes, there is evolving evidence about the health risks. It is important for people to know that e-cigarettes are not a safe alternative to smoking combustible cigarettes.
How Smoking E-Cigarettes Affects Asthma
 A 2016 study of Korean high school students found that using e-cigarettes was linked with increased asthma symptoms and caused school absences. Another study found that people with and without asthma had airway irritation after e-cigarette use, but the airway irritation in people with asthma was a lot worse, and they took twice as long to recover.
A 2016 study of Korean high school students found that using e-cigarettes was linked with increased asthma symptoms and caused school absences. Another study found that people with and without asthma had airway irritation after e-cigarette use, but the airway irritation in people with asthma was a lot worse, and they took twice as long to recover.
Learn more about e-cigarettes including laws, why they are so popular with kids, and additional health and safety concerns.
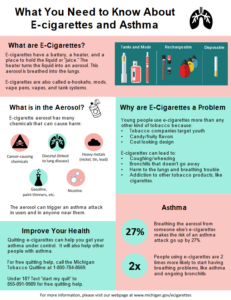
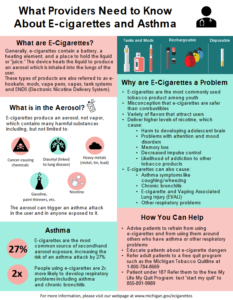
Two infographics from the MDHHS Asthma and Tobacco Programs:
- For healthcare providers to learn more about e-cigarettes and how to help their patients who use them
- For people with asthma and their caregivers to learn more about e-cigarette dangers and where to get help to quit (e-cigarette infographic English) (e-cigarette infographic Spanish)
What is Secondhand Smoke?
Secondhand smoke is smoke from burning tobacco products like cigarettes, cigars, hookahs, and pipes, and the smoke that is exhaled by someone who smokes. There are more than 7,000 chemicals in tobacco smoke, including hundreds that are toxic and about 50 of them that can cause cancer.
Secondhand smoke contains benzene (found in gasoline), butane (use in lighter fluid), ammonia (used in household cleaner, toluene (use in paint thinners), cadmium (used in making batteries), and hydrogen cyanide (used in chemical weapons).
Health Effects of Secondhand Smoke
Every year, more than 41,000 people die of secondhand smoke exposure. Secondhand smoke is unhealthy for everyone but particularly for unborn babies, infants, and children because their bodies are still growing.
Tobacco smoke is a common trigger for asthma, and people with asthma who smoke or are exposed to secondhand smoke have a higher risk of asthma attacks.
In adults, breathing in secondhand smoke can:
- Cause lung cancer.
- Increase the risk of getting nasal sinus cancer.
- Increase the risk for heart attack and stroke.
- Irritates the lungs, leading to coughing, excess mucus, chest discomfort, and poorer lung function.
- Increase eye and nose irritation.
In infants and children, breathing in secondhand smoke can:
- Cause children to develop asthma.
- Lead to more frequent and more severe asthma attacks.
- Increase the likelihood of getting pneumonia and bronchitis.
- Increase the likelihood of developing breathing problems that don’t get better and poor lung function.
- Increase the likelihood of having more middle ear infections.
- Increase the risk of Sudden Infant Death Syndrome (SIDS), which is the main cause of death in infants between one month and one year of age.
- Cause infants to have a low birth weight or be small for gestational age.
Where is the Smoke?
Exposure to secondhand smoke can come from many locations including homes, restaurants, worksites, public places, and vehicles. The greatest exposure for children usually comes in the home. Almost 41% of U.S. children aged (3-11) years are exposed to secondhand smoke in the home (Centers for Disease Control MMWR 2015). In Michigan, 18.6% of adults are exposed to secondhand smoke exposure at home or in a vehicle, as compared to 59.6% of adults in low socioeconomic status households (2020 Michigan BRFSS.)
Pollution levels generated by secondhand smoke in vehicles can rapidly reach dangerously high levels. Ventilating a vehicle fails to protect children inside from the health risks associated with exposure. Similarly, opening a window or smoking in another room does not protect children from secondhand smoke exposure. (CDC)
Secondhand Smoke and the Worksite
Since 2010 Michigan residents and visitors are protected from exposure to secondhand tobacco smoke in all restaurants, bars and businesses (including hotels and motels), thanks to the Dr. Ron Davis Smoke Free Air Law. Click on MDHHS – Michigan’s Smoke-Free Indoor Air Law for more information. For more information on smoke-free worksite policy, please call 517-335-8376.
Secondhand smoke is a class “A” carcinogen, something known to cause cancer in humans. There is no safe level of exposure to a cancer-causing agent. Simply dividing smokers from nonsmokers within the same airspace may cut down exposure to secondhand smoke, but cannot get rid of it.
Workers exposed to secondhand smoke on the job are 20-30 percent more likely to get lung cancer (CDC). Exposure to secondhand smoke can also result in worsened asthma symptoms, poor blood circulation, bronchitis, and pneumonia.
Smokefree Air Law Helps Those with Asthma
A study published in Preventing Chronic Disease, “Racial Disparities in Asthma Hospitalizations Following Implementation of the Smoke-Free Air Law, Michigan, 2002–2012,” studied statewide hospital discharge data from January 2002 through December 2012. After adjusting for age, sex, race, insurance type and month of year, there was an 8% reduction in the population-wide rate of asthma hospitalizations in the 12 months after the implementation of the Smoke Free Air Law (SFA). Whites were found to have a higher annual decrease in hospitalization rates (10.5% vs. 7.8% in blacks) after the implementation of the SFA Law. In the 32 months following implementation of the SFA law, researchers saw a reduction of 3,230 adult asthma hospitalizations, saving approximately $48.6 million in health care costs.
Myths and Misconceptions About Smoking
Myth: If I smoke cigarettes in a separate room in the house, then my family is not being exposed.
Fact: Smoke will travel throughout the house no matter where the cigarette is being smoked. It is like putting chlorine in the shallow end of the pool and expecting the chlorine to not circulate to the deep end. Even ventilation systems in homes cannot filter and circulate air well enough to get rid of secondhand smoke. Going into another room to smoke, opening a window or smoking while children are gone will not fully protect them from the dangers of secondhand smoke.
The Surgeon General Report in 2006 stated that even separately enclosed, separately exhausted, negative-pressure smoking rooms cannot keep second hand smoke from spilling into adjacent areas. (The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General, 2006)
In a July 2001 study in the Journal of American Medical Association, investigators found that brief exposure to small amounts of secondhand smoke can immediately affect the hearts of nonsmokers. The study showed that in as little as 30 minutes of exposure to secondhand smoke, the nonsmokers’ blood flow dropped to the same level as people who had smoked a pack of cigarettes. After short amounts of exposure, secondhand smoke had caused damage to the cells that line the heart and blood vessels, causing them to narrow or constrict. This narrowing can lead to hardening or thickening of the arteries and heart disease.
Myth: Simply separating non-smokers within the same areas, such as a workplace or restaurant, will keep them from being exposed to secondhand smoke.
Fact: Separating smokers from nonsmokers, cleaning the air, and ventilating buildings cannot eliminate secondhand smoke exposure. (The Surgeon General Report, 2006).
The American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), the Preeminent U.S. standard-setting body on ventilation issues, has concluded that ventilation systems cannot remove secondhand smoke from indoor environments. (Environmental Tobacco Smoke: Position Document. Atlanta, Georgia: 2005)
Quitting Tobacco Use
Nicotine addiction is the physical dependence of your body to the powerful chemical nicotine. Quitting tobacco is one of the most important things you can do for your health! If you use tobacco and you want to quit for yourself or for the health of others, help is available.
When planning a quit attempt, consider using any or all of the following:
- Self-help information
- Tobacco dependence treatment (coaching) to understand and change behaviors
- Medication to help ease the discomfort of withdrawal from nicotine. Guide to Free or Reduced-Cost Smoking Cessation Medication (pdf)
A tobacco dependence treatment (or quit smoking) program is an important part of the quitting process. It can increase your chances of quitting for good. The following information can help you choose a tobacco cessation program.
Types of Cessation Programs
- Group Programs
- Telephone Cessation (1-800-QUIT-NOW)
- One-on-one Counseling Programs
- Twelve-step Programs (Nicotine Anonymous)
- Self Help Programs
- Inpatient Programs
- Computer-based/Internet Programs
Guidelines for Choosing a Program to Help You Quit
Different programs work best for different people. When choosing a program, consider things like time, place and coaching methods.
- Choose a research-based program.
- Look around for tobacco cessation courses that may be offered at a local hospital, or through your health plan, the American Lung Association, or the American Cancer Society.
- Ask your doctor, nurse or health plan for suggestions about programs with a good reputation.
- When looking for a program, ask for details about the cost and length of the course.
- Are the presenters trained cessation counselors, and do they have a background in health?
- Will your health plan cover all or part of the cost for attending?
- Look for programs that teach avoidance (staying away from tobacco), stress management, coping, interpersonal and refusal skills. It should also address diet, exercise and other health behaviors.
- Will the program help you decide if you are ready to quit? Will it help you determine your motivation for quitting smoking? Will it help you pick a “quit date”?
- You can improve your success at quitting by choosing a program with courses that have at least four to seven sessions, and are at least 45 minutes long.
- Are refresher courses offered? Or can you drop in on another session if you have a slip or feel a need for some extra support?
Tobacco Use Quitline
Telephone-based cessation counseling provides callers with support and coaching. A call to the Michigan Department of Health & Human Service’s free quit program 1-800-QUIT NOW (784-8669) can help. The program is also available online at Michigan Tobacco Quitline (quitlogix.org). Enrollment is available 24/7 and coaching appointments are made based on your schedule. It provides four or more appointments with a personal health coach work with you to develop your personal plan to successfully quit smoking.
In addition to telephone coaching, participants can also opt into text or email messaging. Qualified enrollees may receive free nicotine replacement therapy. Coaching is available line in English, Spanish and Arabic. Other languages are served through a translation line. Special programs are available for prenatal, American Indian, and behavioral health callers.
For youth who are thinking about quitting smoking or e-cigarettes, a special program is available for them at My Life My Quit. This program is free and available to youth up to age 17.
Prescription and Over-the-Counter Tobacco Cessation Medications
The Food and Drug Administration has approved seven medications to assist smokers in quitting:
Five are nicotine replacement therapies that relieve withdrawl symptoms. They include nicotine gum, patch, nasal spray, inhaler, and lozenge.
The two non-nicotine medications are:
bupropion SR (sustained release), a non-nicotine medication that is thought to decrease the urge to smoke by affecting the same chemical messengers in the brain that are affected by nicotine.
Varenicline, an on-nicotine medication,that works by blocking the pleasant effects of nicotine (from smoking) on the brain.
| Type | Form | Common Brand Name(s) | Availability |
|---|---|---|---|
| Nicotine Replacement Therapy | Gum | Nicorette® | Over-the-counter (OTC) |
| Patch | Nicoderm®, Habitrol®, Prostep®, Nicotrol® | OTC and prescription | |
| Inhaler | Nicotrol® | Prescription | |
| Nasal Spray | Nicotrol® | Prescription | |
| Lozenge | Commit®** | OTC | |
| Bupropion | Pill | Zyban®, Wellbutrin® | Prescription |
| Varenicline | Pill | Chantix® | Prescription |
* Approved by the Food and Drug Administration (FDA) and addressed in the 2008 PHS Guidelines.
Helpful Cessation Web Site Addresses
Other helpful resources are cessation web sites. Here are some websites that offer information about quitting:
American Lung Association
Freedom from Smoking
This cessation program has options for online, phone, and local classes.
Resource Hub for Effective Tobacco Cessation Coverage and Health Systems Change
Key resources, webcasts, and toolkits to help states and the tobacco control community improve tobacco cessation coverage and integration into health systems.
Ask, Advise, Refer to Quit Don’t Switch
One-hour tobacco brief intervention training for healthcare professionals.
Not On Tobacco (NOT)
Vaping and tobacco cessation program designed for teens ages 14 to 19 and taught by a trained and certified adult in ten, 50-minute sessions .
NOT for Me
A self-guided, mobile-friendly online program that leverages the American Lung Association’s Not On Tobacco (N-O-T)® program to help teens break nicotine dependency, whether they vape, smoke or use other tobacco products.
Intervention for Nicotine Dependence: Education, Prevention, Tobacco and Health (INDEPTH)
An alternative to suspension or citation that helps schools and communities address the teen vaping problem in a more supportive way by teaching students about nicotine dependence and how to kick their unhealthy addiction.
Tobacco Basics
A free, one-hour online course including five learning modules designed to lay the foundation in understanding the toll of tobacco use in the U.S.
How To Help People Quit
A free, one-hour online course including four interactive learning modules designed to further enhance understanding of the Lung Association’s core beliefs about tobacco cessation, as well as understanding behavior changes, interventions and treatment needed to help people quit for good.
Mayo Clinic
Residential clinic for quitting tobacco. Site also contains facts, information and research about quitting.
American Cancer Society
Offers quit tobacco resources. 248-663-3454 or 1-800-227-2345 (toll-free).
American Heart Association
Offers printed materials and a special Vaping/ Quit Smoking/ Tobacco page. 1-800-242-8721 (toll-free).
Centers for Disease Control and Prevention (CDC) How to Quit website
has information about free quit tobacco guides, booklets, and fact sheets. CDC also manages a complete website dedicated to helping commercial tobacco users quit at www.smokefree.gov, with special sections for veterans, teens, women, Spanish-language smokers, and people 60-plus. A SmokefreeTXT message program and Smokefree Smartphone apps are available.
Other Important Tobacco Links
Smoke Free Environments Law Project
SFELP provides information, consultation and advice for the Michigan Department of Health and Human Services, local units of government, tobacco control advocates, and communities regarding evidence-based policies and practices to protect Michigan residents from the harmful effects of tobacco. SFELP has operated for over 20 years with the support of the Michigan Department of Health and Human Service’s Tobacco Section.
In that time, the project has addressed a number of issues, ranging from local smoke-free public health regulations and Michigan’s statewide smoke-free law to smoke-free public housing policies, smoke-free policies for parks and beaches, youth e-cigarette use, tobacco use in vulnerable and marginalized communities, and raising the minimum age of sale of tobacco products to 21.
Services for Michigan Employers and Residents
American Lung Association
The Stop Smoking Section includes quitting smoking information, smoking and women and smoking and teens. This site also contains information on their Not On Tobacco (NOT) ten-session tobacco cessation program for teens.
Environmental Protection Agency
Gives information and links to resources about secondhand smoke, gives information on lists of publications about secondhand smoke, and gives basic information about secondhand smoke and how it affects asthma.
Information about Smoking and Cancer
Campaign for Tobacco-Free Kids
Offers current tobacco news, youth action, research and facts, information about your state, links to other useful sites and much more. and facts, information about your state, links to other useful sites and much more.
Center for Disease Control and Prevention
CDC’s Tobacco Information and Prevention Sources (TIPS) offers up-to-date information on major events, such as the Tips from Former Smokers media campaign, a Spotlight category and Tools and Resources category.
