Managing Asthma in Children 12 Years of Age and Adults
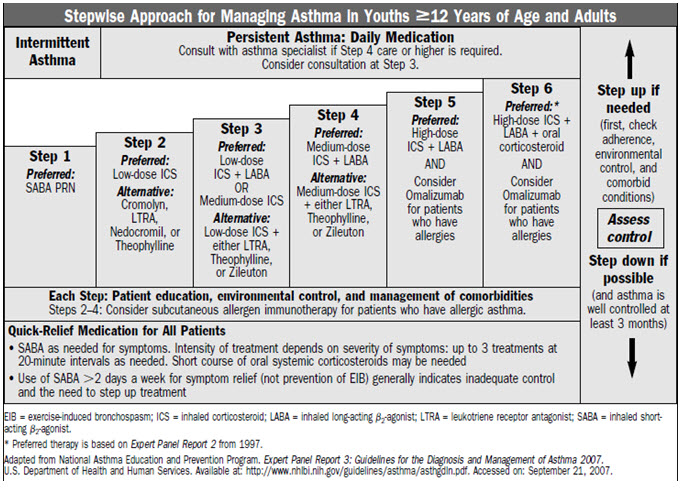
Once a patient has been classified for the level of severity of their asthma, the health care provider can use the stepwise approach to gain or maintain control the patient’s asthma.
Stepwise Treatment Approach
 Notes:
Notes:
- The stepwise approach is meant to assist, not replace, the clinical decision making required to meet individual patient needs.
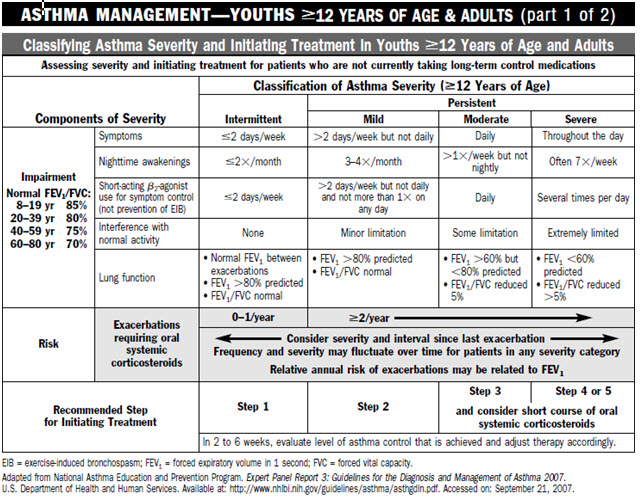
- Level of severity is determined by assessment of both impairment and risk. Assess impairment domain by patient’s/caregiver’s recall of previous 2–4 weeks and spirometry. Assign severity to the most severe category in which any feature occurs.
- At present, there are inadequate data to correspond frequencies of exacerbations with different levels of asthma severity. In general, more frequent and intense exacerbations (e.g., requiring urgent, unscheduled care, hospitalization, or ICU admission) indicate greater underlying disease severity. For treatment purposes, patients who had -2 exacerbations requiring oral systemic corticosteroids in the past year may be considered the same as patients who have persistent asthma, even in the absence of impairment levels consistent with persistent asthma.
Quick-Relief for All Patients
Short-acting bronchodilator: inhaled beta 2-agonist (2-4 puffs) as needed for symptoms. Intensity of treatment will depend on severity of exacerbation. Learn more about quick-relief medications.
Notes:
The stepwise approach presents general guidelines to assist clinical decision making. Asthma is highly variable; clinicians should tailor medication plans to the needs of individual patients.
- A course of oral steroids may be needed at any time and step.
- Patients with exercise-induced bronchospasm should take 2 to 4 puffs of an inhaled beta2-agonist 5-60 minutes before exercise.
- Referral to an asthma specialist for consultation or co-management is recommended for patients requiring step 3 or 4 care. Referral may be considered for step 2 care.
- Learn more about known risk factors for death from asthma.
Gaining Control
The physician’s judgment of an individual patient’s needs and circumstances will determine at what step to initiate therapy. The recommended approach to gaining control of asthma:
- At the onset, give therapy at a higher level to achieve rapid control and then step down to the minimum therapy needed to maintain control. A higher level of therapy can be accomplished by either adding a course of oral steroids to inhaled steroids or using a higher dose of inhaled steroids.
- If control is not achieved with initial therapy (e.g. within 1 month), the step selected, the therapy in the step, and possibly the diagnosis should be reevaluated.
Maintaining Control
Increases or decreases in medications may be needed as asthma control vary over time. The NHLBI guidelines recommend follow-up visits every 1-6 months to monitor the patient’s asthma. In addition, patients should be instructed to monitor their symptoms (and peak flow if used) and adjust therapy as described in their Asthma Action Plan.
 Notes:
Notes:
- The stepwise approach is meant to assist, not replace, the clinical decision making required to meet individual patient needs.
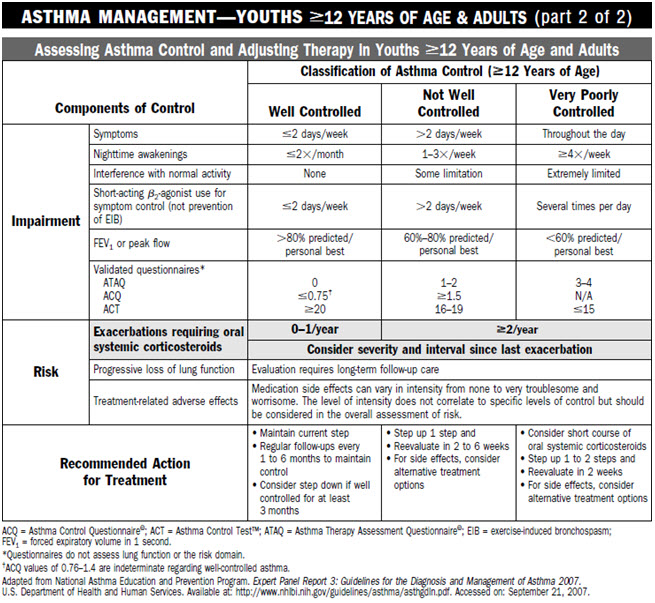
- The level of control is based on the most severe impairment or risk category. Assess impairment domain by patient’s recall of previous 2–4 weeks and by spirometry/or peak flow measures. Symptom assessment for longer periods should reflect a global assessment, such as inquiring whether the patient’s asthma is better or worse since the last visit.
- At present, there are inadequate data to correspond frequencies of exacerbations with different levels of asthma control. In general, more frequent and intense exacerbations (e.g., requiring urgent, unscheduled care, hospitalization, or ICU admission) indicate poorer disease control. For treatment purposes, patients who had -2 exacerbations requiring oral systemic corticosteroids in the past year may be considered the same as patients who have not-well-controlled asthma, even in the absence of impairment levels consistent with not-well-controlled asthma.
- Validated Questionnaires for the impairment domain (the questionnaires do not assess lung function or the risk domain)
- ATAQ = Asthma Therapy Assessment Questionnaire©
- ACQ = Asthma Control Questionnaire© (user package may be obtained at www.qoltech.co.uk or juniper@qoltech.co.uk)
- ACT = Asthma Control Test™
- Minimal Important Difference: 1.0 for the ATAQ; 0.5 for the ACQ; not determined for the ACT.
- Before step up in therapy:
- Review adherence to medication, inhaler technique, environmental control, and comorbid conditions.
- If an alternative treatment option was used in a step, discontinue and use the preferred treatment for that step.
Step Down Therapy
Gradually reduce or “step down” long-term-control medications after several weeks or months of controlling persistent asthma (i.e., the goals of asthma therapy are achieved). In general, the last medication added to the medical regimen should be the first medication reduced.
Inhaled steroids may be reduced about 25 percent every 2 to 3 months until the lowest dose required to maintain control is reached. For patients with persistent asthma, anti-inflammatory medications should be continued. Learn more about long-term controller medications.
For patients who are taking oral steroids daily on a long-term basis, referral for consultation or care by an asthma specialist is recommended. Patients should be closely monitored for adverse side effects. Continuous attempts should be made to reduce daily use of oral steroids when asthma is controlled:
- Maintain patients on the lowest possible dose of oral steroids (single dose daily or on alternate days).
- Use high doses of inhaled steroids to eliminate or reduce the need for oral steroids.
 Step Up Therapy
Step Up Therapy
Asthma classified as not well controlled or very poorly controlled is an indication for stepping up therapy. Before increasing therapy, alternative reasons for poorly controlled asthma should be considered. Referral to a specialist for co-management or consultation may be appropriate. Learn when to refer patients to an asthma specialist.
Recommended Action for Treatment Based on Assessment of Control
| Well Controlled | Not Well Controlled | Very Poorly Controlled |
|---|---|---|
| Maintain current step | Step up 1 step and reevaluate in 2-6 weeks | Consider short course of oral corticosteroids |
| Consider step down if well controlled for at least 3 months | For side effects, consider alternative treatment | Step up 1-2 steps and reevaluate in 2 weeks For side effects consider alternative treatment options |
Before increasing Medications – Assess Reasons for Poor Asthma Control – ICE
- Inhaler technique – Check patient’s technique.
- Compliance – Ask when and how much medication the patient is taking.
- Environment – Ask patient if something in his or her environment has changed.
Is there environmental tobacco smoke in the home? Find out about cotinine levels, which can help track exposure to tobacco smoke and its toxic constituents using a saliva, blood or urine test.
You may also want to consider an alternative diagnosis. Assess patient for presence of other upper respiratory disease.
Adapted from the Practical Guide for the Diagnosis and Management of Asthma, NIH Publication, August 2007, National Institutes of Health, National Heart, Lung and Blood Institute
