Explaining Asthma to a Child
When a child is small, it can be hard to explain what asthma is. Try the
tips below to make this job a little easier. Always use pictures
to help you explain, and ask your doctor for pictures if you
don't have any. You will need to fit these explanations to your
child's asthma symptoms and action plan.
- Talk about how normal lungs work.
- "Your lungs are in your chest. When your lungs are normal, the air goes in and out easy. The tubes inside your body that carry the air in and out of your lungs are round and open and clear."
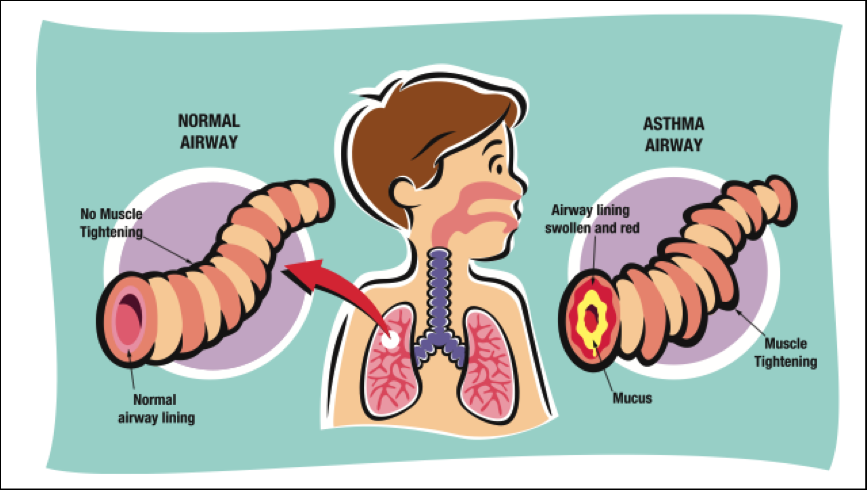
- Talk about what happens during an asthma attack.
- "Because you have asthma, you have twitchy lungs. That means that when you breathe in ____________ (child's trigger), your lungs get all tight, and make thick, sticky stuff called mucus. That's why it's hard to breathe, and you feel like coughing."
- Talk about the medicine they take (fit to child's medication plan).
- Long-term controller medicines: "You need to take some of your medicine every day to keep your lungs from getting tight and making that thick, sticky stuff. Even when you feel good you need to keep taking it, because it helps keep you from having asthma attacks."
- Quick-relief medicines: "When you feel like you are having trouble breathing, we use this medicine to help you feel better fast."
- Valved-holding Chamber/Spacer: "This helps the medicine get into your lungs better. It makes a cloud of medicine inside the tube, then you breathe the
medicine deep into your lungs."
- Nebulizer: "The nebulizer is a machine that makes a mist with your medicine in it. It isn't hot like the steam that comes out of the tea kettle, even though it looks like that. It's really cool like a cloud. When you breathe that mist in, the medicine can go deep in your lungs. This makes it easier to get the medicine you need."
- Talk about going to the doctor.
- "Asthma is a disease that can be serious and tricky. The doctor helps us figure out the best ways to take care of it so that you can play and act just like other kids. We need to visit the doctor pretty often so that he can make sure that you are doing okay with your medicines and aren't having any trouble breathing. He will listen to you breathe and ask you if you have any trouble sleeping or when you play. He will make sure we know all about your medicines and the things that make you have an asthma attack, so we can keep an attack from happening."
- "At the doctor, we will make an Asthma Action Plan, which is a plan for how to take care of your asthma. We will give copies of this plan to _________(list all the people child is with, such as babysitter) so that they know what to do if you have trouble breathing."
- Talk about using a peak flow meter.
- "This is a tool we use to find out how your asthma is doing.
Sometimes it's hard to tell if your asthma is starting to get bad, so we blow into this, and it tells us how fast you
can blow out. That number gives us an idea about how your asthma is doing. We will find the number that is the best you can do
when you're feeling well. Then, when you do this every day, we'll see if the
number is the same, a little or a lot worse. We will think about how you are feeling, and if the numbers are low and
you feel bad, too, we'll do what it says on the action plan, and maybe go see the doctor."
- Talk about triggers (use the triggers that affect your child).
- Exercise: "You know how when you're running around you sometimes feel like it's hard to breathe, and you have to stop or slow down. That's what starts your asthma. We want to keep your asthma under control so you can do everything all of your friends are doing."
- Infections: "When you get a cold, the germs that make you feel yucky also can make your breathing feel tight. That's what starts your asthma."
- Allergies: "You are allergic to____________ (put in child's allergy, such as cats). When you are around ____________ (child's allergy) you breathe in stuff that makes your breathing hard. That's what starts your asthma."
- Irritants: "There are things in the air sometimes that cause people with asthma to start to have trouble breathing. Your asthma starts up when you are around ______________ (put in child's trigger, such as cigarette smoke)."
- Weather: "We've figured out that your asthma is started by the weather sometimes. That's why we always check your peak flow carefully and watch for ____________ (put in child's symptoms) on _________ (type of weather, such as foggy) days. That's what starts your asthma."
- Emotions: "When you are______________ (put in child's emotional trigger, such as laughing or crying) a lot, sometimes you start to feel like you can't breathe. That's what starts your asthma."
- Avoiding triggers: "To keep you from having trouble breathing, we try to stay away
from____________ (child's triggers). Sometimes we can't do that very well, so we make sure that we know what to do when you have trouble breathing. If you know that you are near something that makes your asthma worse, tell a grownup right away."
- Talk about what to do about their asthma attacks (fit to child's
warning signs/symptoms).
- Green zone: "This is when you are feeling good aren't having asthma symptoms. In order to stay in the green zone, we'll keep using the medicine and staying away from your triggers like the doctor tells us to."
- Yellow zone: "When
you _______________ (put in child's early warning signs,
such as looking pale) we know that your asthma is starting so
we'll do what it says to do on the action plan for yellow
zone. For you, that means we _______________ (put in
child's yellow zone actions). If I'm not with you and
you feel like your asthma might be starting, tell an adult
right away. It's much better to take the medicine when you first start
feeling bad than to wait for your breathing to get hard."
- Red zone: "When you feel like you can't breathe very well and your peak flow is really low, tell someone right away. You’ll need to do what your asthma action plan says to do for the red zone, and for you that means _______________ (put in child's red zone actions). Then we'll take you to the doctor or the emergency room. This is a very bad time for your lungs and we need to make sure they get lots of help fast."
Compiled from the experiences of asthma educators across the state of Michigan, 2001, and adapted from the Practical Guide for the Diagnosis and Management of Asthma, NIH Publication No. 97-4053, October 1997, National Institutes of Health, National Heart, Lung and Blood Institute